Would you like a new job? The hours might be difficult, but you will get to meet judges, doctors and people with experiences of disabilities. You might have to get used to severe, crushing blows and knocks in your confidence for things that are not your fault. You may have to get used to judges, doctors and people with experience of disabilities justifiably haranguing you for the actions of others.
A recent parliamentary question has confirmed that the Department for Work and Pensions are recruiting presenting officers- those long fabled people who will turn up at tribunals to represent the decision making power of the Secretary of State. When I was a welfare rights worker the chance of a presenting officer turning up to appeal was somewhere lower than zero. Indeed, the answer confirms that not one presenting officer was recruited between 2012 and 2017, with more than 200 now recruited in 2017.
Now, if you’ve read my blog you’ll know I’ve shown a strong interest in this process and have suggested that the DWP need to be fronting up for appeals- so in a very limited way I support this change. What I want to look at this time is what impact it will have and whether the presenting officers will be allowed the kind of changes that will allow a real impact on decision making across the health related benefits.
But what will the role of presenting officers be? They’re very lucky (in one way) in that their role is government by a statutory instrument (a piece of secondary legislation) setting out their duties (and everyone else’s) in an appeal. There’s also, for universal credit and personal independence payments, a whole chapter on the decision makers guide which goes into great detail about what they should be doing. Let’s try and precis them!
Presenting officers aren’t lawyers- but they don’t necessarily need to be. What they need to have is a very good understanding of the benefit system and the operation of the tribunal. Their job is to:
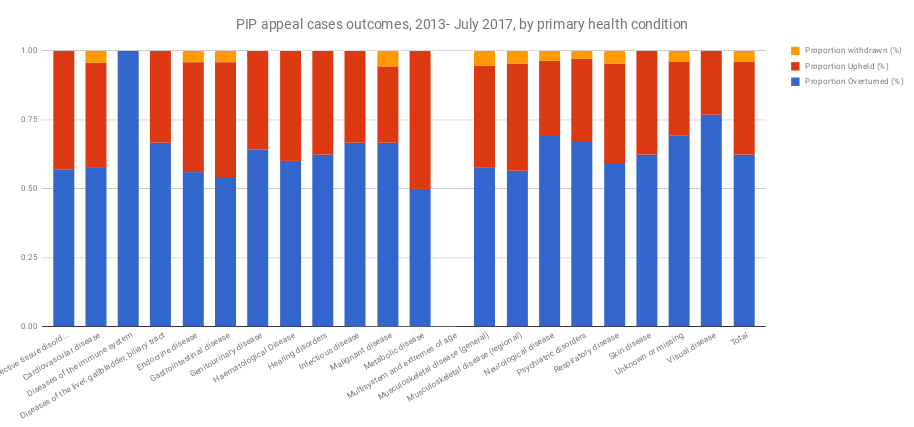
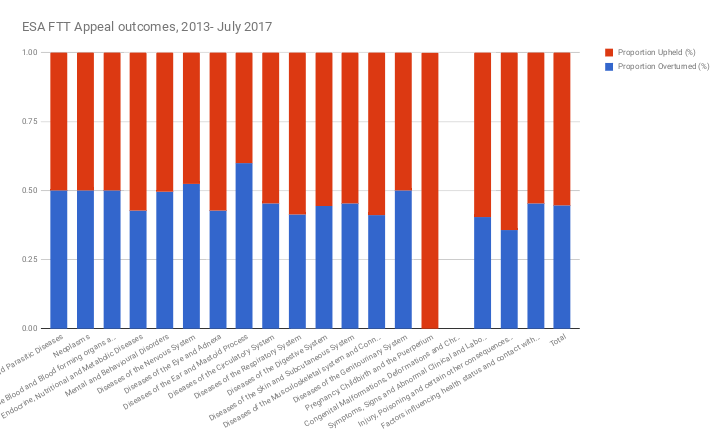
- Check that the original decision was right in light of the evidence in hand. If it isn’t (and do remember than two thirds of ESA decisions are overturned at Tribunal) then they can and should change the decision- at the very least sending it back to the decision makers. For universal credit and personal independence payments the decision makers guide is very clear that the presenting officer must satisfy themselves that the decision is right before they attend the appeal.
- Attend the appeal and put explain the Secretary of State’s decision, including how the evidence has been weighed. The presenting officer can ask questions of other people present (including the claimant) but these shouldn’t be combative and should be focused on understanding any disagreement in the written submissions. In benefit appeals people aren’t there to win or lose, but to find the truth through collaboration. I know that sounds otherworldly, but it is an important point- if you do a victory dance at the end of an tribunal you are likely to be rebuked pretty quickly!
- After the appeal- reflect, consider and think on what happened and what could have been done better. In a way, this is simply number 1 restated- the next time they have a similar case they have to ask themselves if they should be taking it at all to appeal.
Now, anyone who has spent any time working with benefit claimants will know that there is often a gap between what the legislation and guidance says and what actually happens on the ground. If you’ve ever had to sit there (usually on the phone) whilst a decision maker pulls up the guidance (trying to talk legislation on the phone is often pointless), turns to the page you are talking about, looks at the paragraph you are talking to, reads it through, tries to justify their existing argument then grudgingly accepts you are correct will know that what happens on paper and in real life are two different things.
So what am I worried about? Primarily, that 1 and 3 above won’t happen. The presenting officers will not use their powers to spot cases that don’t stand a chance of winning, will go to the appeal, the decision will be overturned by the tribunal and they won’t learn anything about why this was. This is perhaps unfair, or even cynical. Perhaps I should give it a chance before I predict doom?
Well, in any case it won’t be long. For ESA alone the number of appeals attended by a presenting officer has shot up since April 2017. The number of attendances between April and December last year is nearly 10 times the total number for the year before, which we know again due to a parliamentary question! Perhaps in their early months presenting officers are there to comprehend and understand, but you’d hope that pretty soon they will get to grips with which cases have a chance at having the decision upheld and which should be overturned quickly now to save the bother of a failed appeal.
As they get better at this you would hope that the original decision makers understand which decisions are unlikely to get past the presenting officers (ie. those people who have to try and make the case) and start amending their decisions. You’d also hope that presenting officers would get better at spotting marginal cases (where their presence may make a difference) and start attending these- rather than being sent on fools errands either by decision makers or even worse an algorithm telling them which to attend.
If this change to the system worked perfectly it could have a huge impact. When I look at the stats in the next few months I’ll be looking for some big changes. If decision makers know they have to make fully reasoned cases then a lower proportion may be turned down in the first place, followed by a lower proportion of appeal cases making it to the tribunal (as they have been sent back by presenting officers) and finally a higher proportion of decisions being upheld (ie. staying the same) rather than overturned as the unwinnable cases have been weeded out and presenting officers have been able to argue the case in some cases successfully.
If the system doesn’t work perfectly the presenting officers will be receiving payment for turning up and being told off, which isn’t fair on them or anybody else. I’ll be looking through the stats as soon as they come out, and so should you.
What I’d prefer to see, instead of a separating out decision making into different sections is decision makers having responsibility for the whole process, holding onto a case and having to present it at appeal. As I’ve spoken about before, the process of decision making is becoming incredibly mechanistic. Indeed, some good soul has been able to winkle out of the DWP their set lines for appeals. Yes, we all knew they existed, but how can individual people with their individual health needs be reduced to set words? If decision makers actually saw what happened in cases that go to appeal they may think twice before making a sloppy decision a second time.
But, as a final point, all of this is essentially moot because of one thing. Mandatory reconsideration still means that a huge proportion of people being turned down for health related benefits are not formally appealing them. Whilst this is the case we won’t know if these claimants are genuinely entitled to benefit. I have no reason to believe those decisions aren’t as second rate as those getting to appeal.
So let’s hope the presenting officers make a big difference, far bigger than their relatively small numbers may show. But that will only happen if they are empowered to act and able to get the department to understand how obvious the failures of decision making are to tribunals and independent observers.